In 1992, the U.S. Army began the practice of retiring health records to the U.S. Department of Veterans Affairs (VA) when military personnel left active service. By 1998, the other branches of the U.S. military followed suit. It’s been a rocky road since. Beginning in 1998, the VA and the U.S. Department of Defense (DoD) had been working on developing an integrated system for the sharing of electronic health records (EHRs) between the two agencies. This effort came to an end by February 2013 without an integrated system after $564 million had already been spent on the project. At that time, the two agencies agreed to a plan which would have them create separate EHR systems which were interoperable, allowing for the timely sharing of health records.
Interoperability between the two agencies, however, has also proved to be thorny. The VA announced this April that its EHR system had reached certification for interoperability, months after the DoD had reached the same milestone, but investigators at the U.S. Government Accountability Office (GAO) reached a different conclusion. A recent GAO report indicated that, although the goal of true interoperability between the agencies can be met within two years according to agency planning, the two systems weren’t truly interoperable. As the GAO noted, medical images such as X-ray images and CT scans could not be shared via the Joint Legacy Viewer (JLV) used by the two agencies to share records.
Furthermore, the inadequate nature of IT used throughout the VA has been well-noted in recent years by news outlets, although it’s certainly not the only federal agency with such a problem. The VA’s scheduling scandal which unfolded throughout 2014 threw a bright light on the antiquated nature of the agency’s IT. Government reports auditing the VA’s actions found troubling lapses in data integrity and information governance. Other reports indicated that the Obama Administration was made aware of problems stemming from an antiquated scheduling system as early as 2008. In some instances, the VA was using software which was almost 30 years old.
It’s in this environment, heavily tinged by the recent GAO report, that a subcommittee of the U.S. Senate Committee on Appropriations came together to take a closer look at what was being done by the VA and the DoD to reach true interoperability. The hearing, titled Hearing to Review the VA Electronic Health Record Network (VistA), was held by members of the Military Construction, Veterans Affairs, and Related Agencies subcommittee. The Veterans Health Information Systems and Technology Architecture (VistA) is the health IT system put in place by the VA to track inpatient and outpatient data involving military veterans.
 Private actors have been getting more involved with the world of EHRs. The patent portfolio analysis tools at Innography show that U.S. patent grants in that sector shot up sharply from three patents in 2009 up to 68 patents in 2014. The three companies with
Private actors have been getting more involved with the world of EHRs. The patent portfolio analysis tools at Innography show that U.S. patent grants in that sector shot up sharply from three patents in 2009 up to 68 patents in 2014. The three companies with 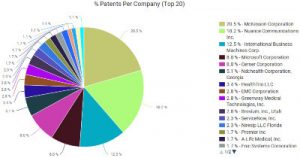 the largest portfolios in this field are McKesson Corporation (NYSE:MCK) of San Francisco; Nuance Communications (NASDAQ:NUAN) of Burlington, MA; and patenting powerhouse IBM (NYSE:IBM)
the largest portfolios in this field are McKesson Corporation (NYSE:MCK) of San Francisco; Nuance Communications (NASDAQ:NUAN) of Burlington, MA; and patenting powerhouse IBM (NYSE:IBM)
The subcommittee’s chairman, Sen. Mark Kirk (R-IL), noted that 250,000 military service members leave the DoD every year, a rate of about 700 people per day. “Whenever a soldier, sailor or airman leaves active duty and becomes a veteran, we should have 100 percent seamless transmission of their health record to the VA,” Kirk said. He added that creating an open-source industry standard for medical record sharing along with data analytics for predicting negative health outcomes could be of great benefit to veterans.
“We live in the 21st century and our IT systems should reflect that,” argued Sen. Jon Tester (D-MT). He noted that, in his home state of Montana, scheduling difficulties remained a top complaint among veterans. Although the day’s hearing focused on electronic health records at the VA, that was merely one area among many at the VA which could focus its efforts at modernization, citing concerns over cybersecurity and scheduling. “Electronic record sharing is a great asset for both clinicians and patients, but only if the veteran can get an appointment in the first place,” Tester said.
 Speaking on behalf of technology affairs at the VA was LaVerne H. Council, assistant secretary for information and technology and chief information officer at the VA. She spoke to the efforts to increase both transparency and accountability at that agency in terms of IT initiatives. Cloud-based services developed by commercial interests were one way Council noted that the VA could source IT in a way that allows the agency to consolidate its infrastructure. Council added that the VA has shown the recent ability to incorporate recommendations in recent years from its own Office of Inspector General (OIG), such as standardizing its device policy and addressing critical cybersecurity risks.
Speaking on behalf of technology affairs at the VA was LaVerne H. Council, assistant secretary for information and technology and chief information officer at the VA. She spoke to the efforts to increase both transparency and accountability at that agency in terms of IT initiatives. Cloud-based services developed by commercial interests were one way Council noted that the VA could source IT in a way that allows the agency to consolidate its infrastructure. Council added that the VA has shown the recent ability to incorporate recommendations in recent years from its own Office of Inspector General (OIG), such as standardizing its device policy and addressing critical cybersecurity risks.
Oversight from the GAO was brought to the day’s panel by Valerie C. Melvin, the GAO’s director of information management and technology resources issues. She noted three specific concerns which she believed could hinder the development of a truly interoperable EHR system between the VA and the DoD. These included a lack of outcome-oriented goals for achieving interoperability between the agencies and costly technology duplication which could occur through the VA’s modernization efforts. Melvin also noted that the VA had yet to substantiate its claim that it solo development of its system would be less costly than joint development with the DoD.
“Health data interoperability is essential in improving care,” said Dr. Lauren Thompson, director of the DoD/VA interagency program. Thompson said that her work involved engagement with the Office of the National Coordinator within the U.S. Department of Health and Human Services (HHS). Her office works to identify and map national standards associated with the DoD’s and the VA’s separate systems and she felt that significant progress had been made in recent months.
 The JLV which the VA and the DoD developed to meet its interoperability goal was scrutinized during questioning leading to different views on what interoperability between the two agencies meant. David Waltman, the VistA evolution program executive and senior advisor to the undersecretary for health at the VA, argued that the agencies had met the interoperability goal as they were able to exchange 25 domains of standardized data through the JLV dashboard viewer. Although medical images were not included in the data exchange as of yet, clinicians and other medical professionals would be able to see written notes of the medical reports accompanying such images. Image sharing would be available in a future edition of the JLV, he added; Council later pegged the time frame on that release as coming by this September. This, however, didn’t satisfy the definition of true interoperability among subcommittee members. “It’s interesting that you would say that the notes are more important than the pictures,” Tester said. “I’m not a doctor, but do you ever do a surgery and not look at pictures?”
The JLV which the VA and the DoD developed to meet its interoperability goal was scrutinized during questioning leading to different views on what interoperability between the two agencies meant. David Waltman, the VistA evolution program executive and senior advisor to the undersecretary for health at the VA, argued that the agencies had met the interoperability goal as they were able to exchange 25 domains of standardized data through the JLV dashboard viewer. Although medical images were not included in the data exchange as of yet, clinicians and other medical professionals would be able to see written notes of the medical reports accompanying such images. Image sharing would be available in a future edition of the JLV, he added; Council later pegged the time frame on that release as coming by this September. This, however, didn’t satisfy the definition of true interoperability among subcommittee members. “It’s interesting that you would say that the notes are more important than the pictures,” Tester said. “I’m not a doctor, but do you ever do a surgery and not look at pictures?”
JLV is also currently incapable of incorporating analytics which could aid in veterans health outcomes. At points throughout the hearing, Kirk noted the current availability of analytics related to sepsis and suicide prevention which could have real benefits for veterans. According to Waltman, that would require the additional development of an enterprise health management platform (EHMP) which could integrate data with algorithm analytics. Although Waltman expected the EHMP to be operational by the middle of the 2018 calendar year, he cautioned to say that the platform might not be useful to every case instance of veteran care by that time.
“The reality is there is no system that can support both DoD and the VA at the same time,” Council said. “It will not scale.” This was challenged by subcommittee member Sen. Shelley Moore Capito (R-WV), who noted that private companies such as Amazon don’t have such issues with scalability. Council countered that the dual objectives of clinical management and clinical operations at the same time made such scaling difficult.
Focusing on the scheduling scandal fallout from 2014 was Sen. Tom Udall (D-NM), who asked about the changes which have been made to avoid the same kind of previous manipulation of the system. Council noted that the VistA Scheduling Enhancements (VSE) product developed by the VA tracks any changes which have been made to scheduling. She also discussed the potential of mobile app-based solutions for telemedicine which could help get medical treatment information to veterans in a more timely fashion.
Despite all of the work done at the VA to address interoperability, it seemed clear that much more work remained. Council, who started at the VA about a year before the hearing, said that she was surprised upon joining the agency at the number of custom IT systems which reached 800 applications at the VA, many of which used old architecture. As Kirk noted, that high number would make the VA one of the largest software developers in the country, and that wasn’t the VA’s core competency. Kirk later added that, as this subcommittee was the only one with jurisdiction over both the VA and the DoD, this subcommittee had a unique obligation to address these problems.

![[IPWatchdog Logo]](https://ipwatchdog.com/wp-content/themes/IPWatchdog%20-%202023/assets/images/temp/logo-small@2x.png)


![[Advertisement]](https://ipwatchdog.com/wp-content/uploads/2024/04/Patent-Litigation-Masters-2024-sidebar-early-bird-ends-Apr-21-last-chance-700x500-1.jpg)

![[Advertisement]](https://ipwatchdog.com/wp-content/uploads/2021/12/WEBINAR-336-x-280-px.png)
![[Advertisement]](https://ipwatchdog.com/wp-content/uploads/2021/12/2021-Patent-Practice-on-Demand-recorded-Feb-2021-336-x-280.jpg)
![[Advertisement]](https://ipwatchdog.com/wp-content/uploads/2021/12/Ad-4-The-Invent-Patent-System™.png)







Join the Discussion
No comments yet.